Bacterial communities cause inflammation of the gut
Novel mechanism for Crohn’s disease uncovered
It has already been shown that the community – or microbiota – of intestinal bacteria are involved in a number of illnesses. The microbiota can lead to IBD such as Crohn’s disease and ulcerative colitis, but also to diabetes and obesity. However, it is often not clear whether the modified intestinal microbiome is the cause or a consequence of the disease.
Researchers at Technische Universität München (TUM) have now shown that an unfavorable configuration of bacterial networks in the gut really can cause inflammation. As part of the study, they transplanted the intestinal microbiome from sick animals into the intestines of germ-free mice. These mice developed symptoms specific to Crohn’s disease in their small intestine.
“Although we used mice that had an increased genetic disposition towards Crohn’s-type inflammation, they did not develop symptoms until we implanted the intestinal bacteria of affected animals,” explains Prof. Dirk Haller, TUM Chair of Nutrition and Immunology.
Dysbiosis: a cause of chronic inflammation
One key finding in the study was that chronic IBD is not caused by individual types of bacteria. “It has a lot more to do with the bacterial communities present,” says Haller. “It would appear that some combinations of bacteria are ‘dysbiotic’ – or imbalanced – and their characteristics can now be explained.”
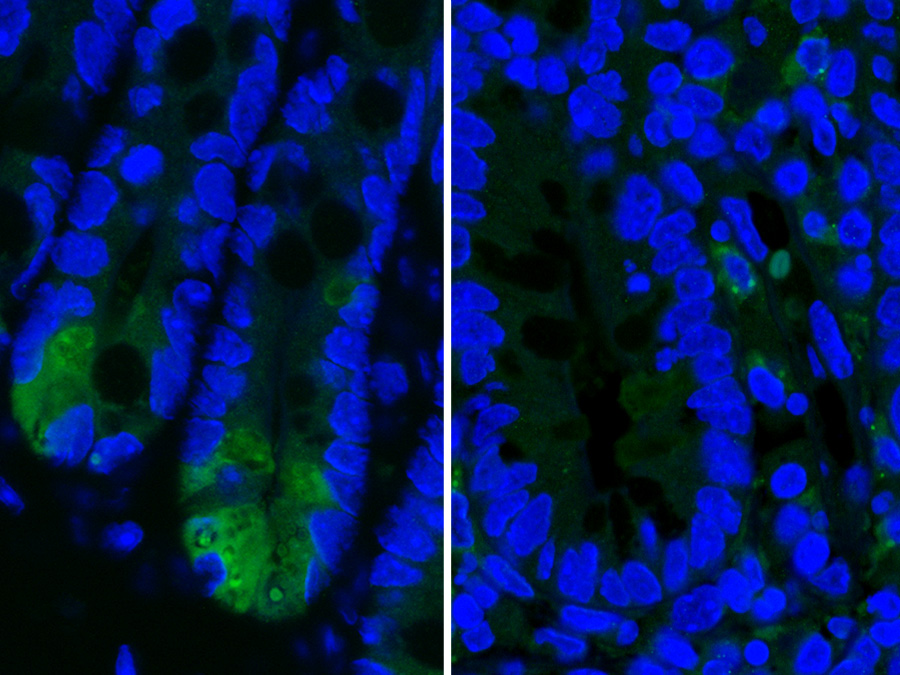
The research team was also able to shed more light on the role of Paneth cells – a type of cell found in the epithelial lining of the small intestine. These glandular cells play a role in the gut’s immune defense. It has been known for a while that these cells die in cases of Crohn’s disease – but it was not clear whether this cell death triggers the disease or microbial imbalance.
The results of the study indicate that the loss of function in Paneth cells is a result of the inflammation, rather than a cause.
Continued development of an unusual treatment
The research team hope that their findings can help increase the range of treatments available for Crohn’s disease. The disease is relatively common: in the developed world, around 40 in 100,000 people will develop Crohn’s disease. In Germany, 350,000 people are thought to suffer from the condition.
For many patients, medication only provides short-term relief. “In most cases, the inflammation returns after a time,” says Haller. “Stool transplants have already proven effective for a number of intestinal diseases. However, this unusual treatment has yet to deliver conclusive results in patients with Crohn’s disease and ulcerative colitis. The findings from our study will help provide a scientific basis for improving this approach – and then it could work.”
----
The study was funded by the German Research Foundation (DFG) as part of their 1656 priority program and HO2236/8-1 program. It also received backing from the Konrad Adenauer Foundation.
Publication:
Dysbiotic gut microbiota causes transmissible Crohn’s disease-like ileitis independent of failure in antimicrobial defence; Monika Schaubeck, Thomas Clavel, Jelena Calasan, Ilias Lagkouvardos, Sven Bastiaan Haange, Nico Jehmlich, Martin von Bergen, Aline Dupont, Mathias Hornef, Marijana Basic, André Bleich, Dirk Haller; Gut Published Online First; DOI:10.1136/gutjnl-2015-309333
Contact:
Prof. Dr. Dirk Haller
Technische Universität München
Chair of Nutrition and Immunology
phone: +49 8161 71-2026
dirk.haller@tum.de
www.wzw.tum.de/bflm
Technical University of Munich
Corporate Communications Center
- Barbara Wankerl
- barbara.wankerl@tum.de
- presse@tum.de
- Teamwebsite