Diabetes research
How does friendly fire happen in the pancreas?
Type 1 diabetes is an autoimmune disease in which the body destroys its own beta cells in the pancreas.* Researchers are still seeking to find out what causes this malfunction of the immune system in order to intervene therapeutically in the processes. A team led by Dr. Carolin Daniel, group leader at the Institute of Diabetes Research (IDF) of Helmholtz Zentrum München, has now discovered a further piece in solving this puzzle.
“For the first time, we were able to show that in the affected children an increased number of specific immune cells are found in the blood at the beginning of the autoimmune response,” said Daniel. She and her team had previously analyzed blood samples of children in a biobank established by Professor Anette-Gabriele Ziegler of TUM and director of the IDF, within the framework of large-scale cohort studies.
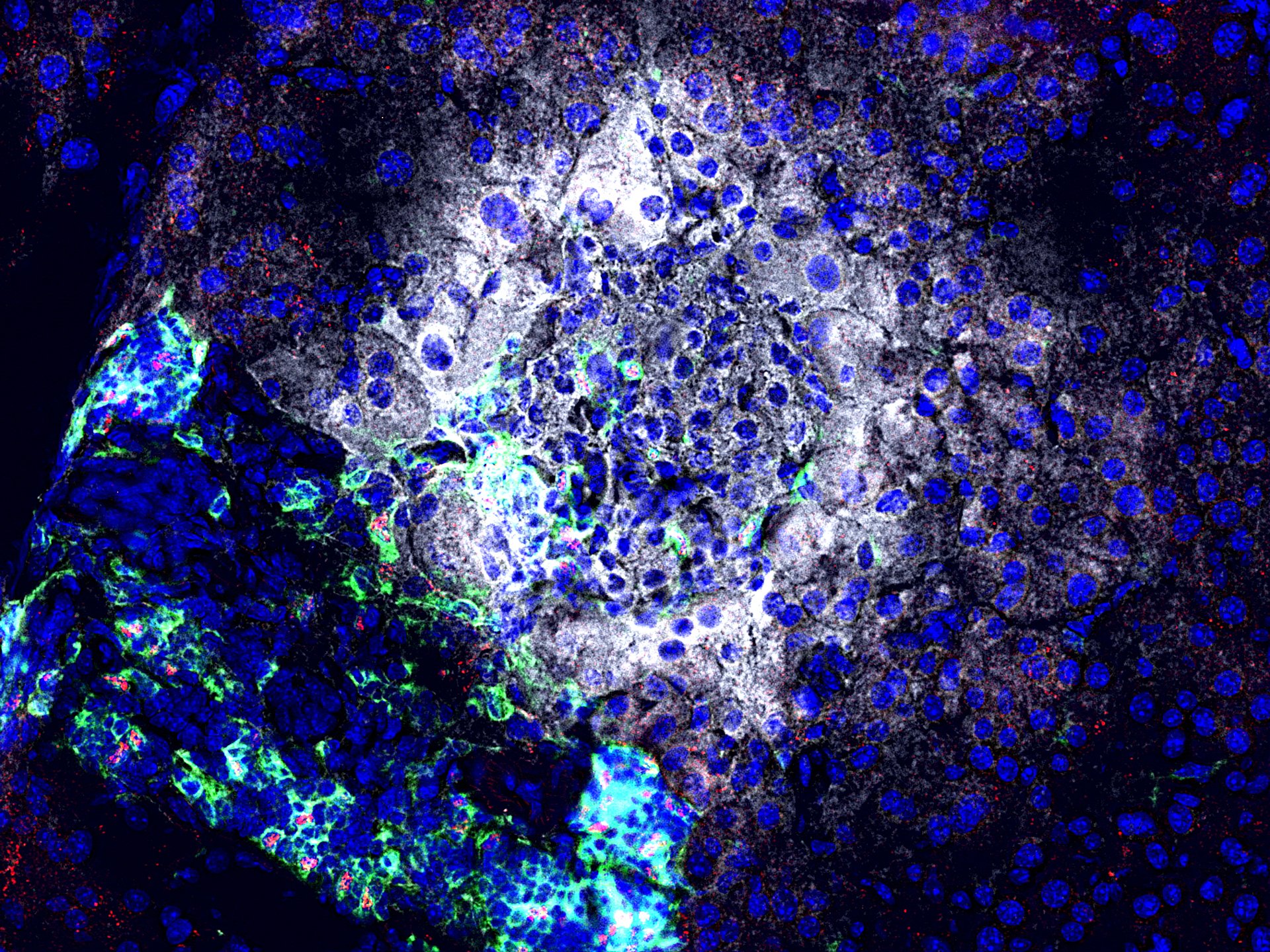
According to the authors, these special immune cells are so-called insulin-specific T follicular helper cells (TFH). They appear in the lymph nodes, among other organs, and initiate attacks of the immune system by promoting the production of antibodies by B cells. Now the scientists have found increased frequencies of these cells in samples of children with recent onset of islet cell autoimmunity – an early stage of type 1 diabetes.
In the search for the causes of the increase in TFH cells during autoimmune activation in children, the scientists discovered a previously unknown signaling pathway. “Our analyses showed that a molecule called miRNA92a** triggers a chain of molecular events, which ultimately leads to the increase in these immune cells,” said IDF doctoral student Isabelle Serr, explaining the complex mechanism. “In particular, during this process, miRNA92a interferes with the formation of important signaling proteins such as KLF2 and PTEN.”
Use in therapy and diagnostics
To check whether this newly discovered mechanism is suitable for therapeutic intervention, the scientists investigated the effect of a so-called antagomir, which specifically binds to miRNA92a molecules and blocks their effect. In an experimental model of type 1 diabetes and in the humanized model, this treatment resulted in a significantly lower autoimmune response.
“The targeted inhibition of miRNA92a or the downstream signaling pathway could open up new possibilities for the prevention of type 1 diabetes,” said Professor Ziegler. "Furthermore, the insulin-specific TFH cells could serve as biomarkers to determine the treatment success of the insulin vaccinations we perform."
Glossary
* In type 1 diabetes, the insulin-producing cells in the Langerhans islets of the pancreas are destroyed because they are attacked by the body’s immune system (formation of islet autoantibodies against structures of the beta cells). As a result, the body can no longer be adequately supplied with insulin. If the destruction of the beta cells exceeds a certain degree, the disease becomes manifest and blood glucose levels rise due to insulin deficiency.
** microRNAs (miRNAs) are noncoding RNAs which play an important role in gene regulation and in particular in the inactivation of genes. In general, they have a size of 21 to 23 nucleotides, so they are very short – hence the name.
Publication:
Serr, I. et al. (2016). miRNA92a targets KLF2 and PTEN signaling to promote human T follicular helper precursors in T1D islet autoimmunity, , DOI: doi/10.1073/pnas.1606646113
ContaCt:
Professor Dr. Anette-Gabriele Ziegler
Technische Universität München
Klinik und Poliklinik für Kinder- und Jugendmedizin
anette.ziegler@tum.de