Can continuous monitoring provide protection for patients?
In-ear sensors to help in fight against COVID-19

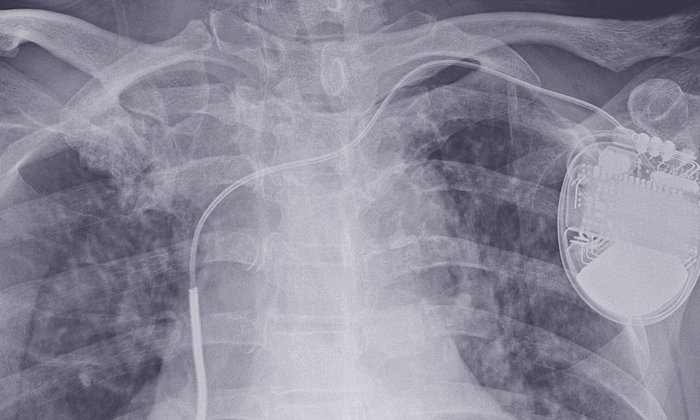
The illness caused by the new coronavirus, SARS-CoV-2, can be roughly divided into two stages. During the first stage, in which symptoms are not acute, infected individuals can generally remain at home. In serious cases, this is followed by a second stage with worsening symptoms in which some patients develop severe pneumonia. "In these cases, patients must be admitted to a hospital as quickly as possible. The sooner they receive good medical treatment, the better the prognosis," explains Prof. Georg Schmidt, the head of the Biosignal Analysis Working Group at TUM’s university hospital Klinikum rechts der Isar.
Prof. Schmidt and his team now want to assess whether a high-tech solution – specifically, an in-ear wearable sensor – can speed up the detection of worsening symptoms in COVID-19 patients. They also hope that prompt treatment will ease the workload of intensive care units by eliminating the need for intensive treatment, including mechanical ventilation, in some cases.
Timely intervention in case of deteriorating symptoms
Persons infected with COVID-19 in Munich are currently contacted by the city's Department of Health and Environment (RGU) as soon as possible after test results are available. RGU asks patients about their health status via telephone every day and offers advice. Anyone who is tested positive can contact a 24-hour telephone service organized by RGU in the event of symptoms, which will come to their home if necessary and organize transport to hospital if necessary. To date, only around 13% of those infected develop severe symptoms and require inpatient treatment.
“Currently, first-stage patients are instructed to take their temperature at home, engage in self-monitoring and to call the health department or their family doctor in case of certain symptoms,” explains Georg Schmidt. “This harbors various uncertainties: The temperature must be measured accurately, the patient has to decide whether to contact a doctor and a decision has to be made whether to admit them to hospital. This can result in delays. We hope that with continuous telemonitoring of biodata and a rapid response when the patient's condition worsens, we can significantly improve the prognosis.”
In-ear-sensors instead of smartwatches
Along with core body temperature, the monitoring will include the patient's blood oxygen saturation, respiration rate and pulse. A composite score, or “polyscore”, will also be calculated several times a day. This indicates how well the body is compensating for the effects of the disease.
Prof. Schmidt has been cooperating with cosinuss, a Munich-based start-up that originated with a doctoral thesis topic at TUM, for some time. The company's in-ear wearable sensors use optical processes, among other technologies, to capture biodata. “These devices can measure all of the parameters we need and transmit them to a small computer via a Bluetooth connection. From there they are forwarded to our central office for analysis in compliance with data protection regulations,” says Georg Schmidt. “A study that we conducted a few months ago on another topic showed that the elderly in particular are at ease with these sensors.”
Close cooperation between science, first responders and the health department
The success of the current study will depend to a large extent on the close cooperation of various parties. Possible participants – COVID-19 patients over 60 years of age living in home isolation in Munich – will be identified through the Munich Department of Environment and Health and can volunteer for participation. Under a doctor's supervision, a team of specially trained medical students in a “control center” at Klinikum rechts der Isar will track the monitored data around the clock. Patients will be reported directly to first responders in case the data, checked against pre-defined parameters, indicate that their condition is deteriorating. This will ensure that they can be transported to a hospital without delay.
“I hope that the research project can provide additional safety for older study participants who stay at home with Covid-19 disease and mild symptoms and do not need hospital treatment. Especially for elderly people living alone, it can be a decisive advantage to ensure automatic permanent monitoring,” said Stephanie Jacobs, head of the Munich health department, welcoming the study.
“We're delighted that we were able to get the health department, the first responders and the Ministry of Science on board so quickly,” says Georg Schmidt. The Munich data will be compared with data from a comparable urban center in Germany where this form of monitoring is not used. The pilot phase of the study, in which processes and structures are being optimized, began on Wednesday, April 15. The first sensors are expected to be issued from the beginning of next week.
A quick start thanks to generous donations
In order to enable the study to start as soon as possible in the current times of crisis, the TUM University Foundation relied on the generous support of its circle of patrons and sponsors. Within a few days, almost 500,000 euros were raised. “By providing unbureaucratic support for this health-related research project, the private donors and sponsors are showing themselves to be socially responsible role models for our society,” says Prof. Thomas F. Hofmann, President of TUM and Chairman of the Board of the TUM University Foundation. “I am particularly grateful for their active commitment to improving the survival chances of Covid-19 patients.”
Frequently asked questions for patients:
Who are the potential study participants?
The study will track COVID-19 patients who are Munich residents and over 60 years of age. They must have a confirmed diagnosis and require neither intensive care nor mechanical ventilation at the time of enrolment. To obtain usable data, the study needs at least 1,200 participants.
Can I volunteer for the study?
Yes, it is expected that from the beginning of next week, the Department of Health and Environment of the City of Munich will send out a flyer with the contact details of the study team at the Klinikum rechts der Isar, together with general information to all persons eligible for the study. Those interested can contact the Klinikum rechts der Isar using the data provided and participate in the study on a voluntary basis. Other persons cannot participate in the study.
There is a central telephone number for inquiries: +49 89 4140 8585.
Technical University of Munich
Corporate Communications Center
- Paul Hellmich
- paul.hellmich@tum.de
- presse@tum.de
- Teamwebsite
Contacts to this article:
Prof. Dr. Georg Schmidt
Technical University of Munich (TUM)
Klinikum rechts der Isar
Clinic and Policlinic for Internal Medicine I, Cardiology
Tel: + 089 289 22731
gschmidt@tum.de