A new look at the brain’s immune system
Using organoids to learn about autism

In the brain, microglia perform such functions as engulfing damaged nerve cells and removing the debris. They can also promote the growth of neurons. As a result, they play an important role in the development of the brain and in diseases of the nervous system.
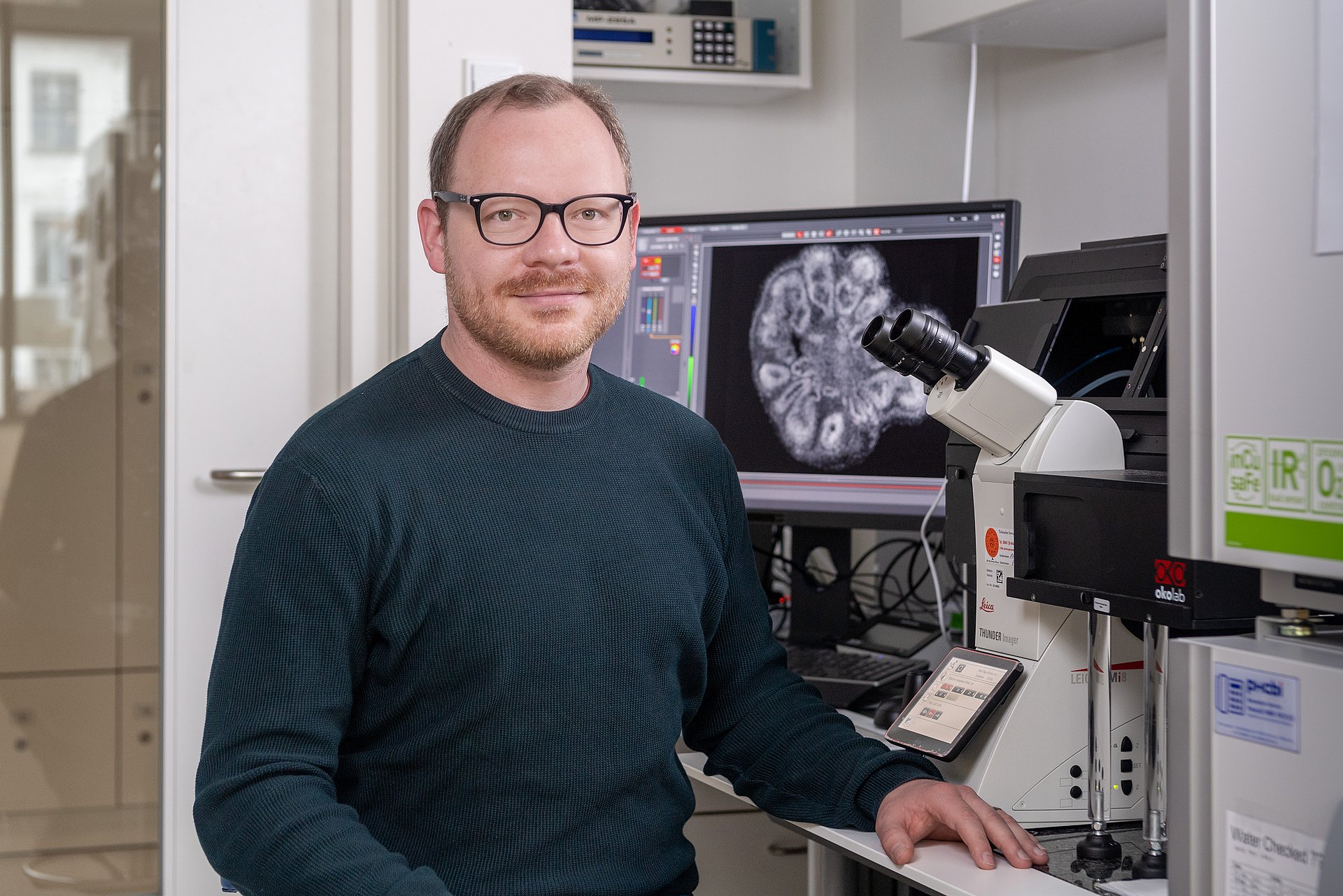
Until now, many aspects of how microglia function have remained unknown. This is partly because their behavior under laboratory conditions is fundamentally different than in the human body. An international research team in which Simon Schäfer, Professor for Advanced Organoid Technologies for Mental Health Research at the Technical University of Munich (TUM), has made decisive contributions, describes an approach to this problem in the journal Cell.
Creating microglia and organoids from stem cells
“Outside of the brain environment, microglia lose almost all function and meaning,” says Prof. Rusty Gage, senior author and holder of the Vi and John Alder Chair for Research on Age-Related Neurodegenerative Disease at the Salk Institute in California. “We knew that if we found a way to replicate the human brain environment in an organoid in order to study human microglia, then we would finally have a tool for examining how the healthy and diseased brain influence microglia and, reciprocally, how healthy and diseased microglia influence the brain.”
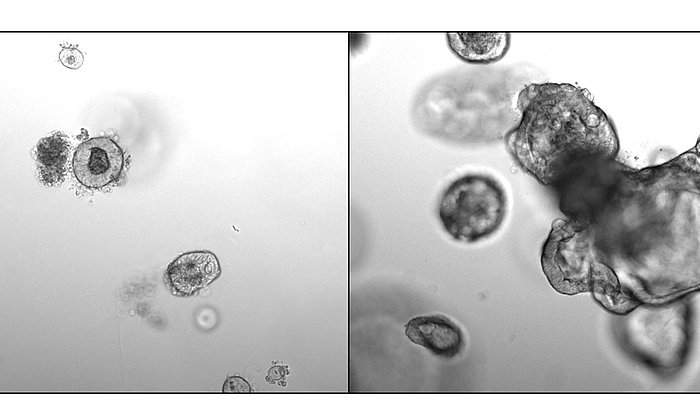
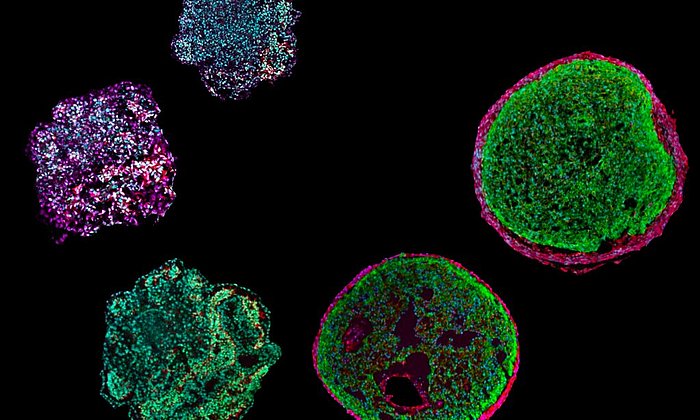
The team developed a process for producing microglia from human pluripotent stem cells. Using these stem cells, the researchers were also able to produce an organoid with approximately 5 millimeters in diameter. In contrast to previous brain organoids, it permits the modelling not only of the initial stage of brain development, but also subsequent stages. This is an important prerequisite for studying diseases that occur later in life.
A three-dimensional cell system
“Organoids are often described as miniature versions of organs,” says Simon Schäfer. “But that creates false associations in this context. When we think about the brain, we think about consciousness, sensations and thought. Our organoids are not able to do that. Nor is that our intention.” Although organoids contain neurons that communicate with one another, he explains, they lack the networking between different areas that is necessary for thought and consciousness. “More realistically, we should think of them as three-dimensional cell systems that we use to model aspects of brain development,” says Schäfer.
Imitating processes in the body
As the next step the team developed a process to seed the stem cell-derived microglia into organoids. This made it possible to model an additional process in the development of the brain: microglia do not move into the area that later forms the brain until around the fifth week of pregnancy.
Until now, microglia or organoids in a petri dish did not behave in the same way as in the human body. However, the team was able to implant the organoids into mice. In a living organism the microglia behaved like their counterparts in the brain. They multiplied and were able to eliminate damaged neurons in the organoid. “We’re now trying to find out how we can get our organoids in the petri dish to behave like those in the body,” says Simon Schäfer.
Organoids from stem cells of autistic patients
With the new organoid system, the researchers want to learn more about how the brain develops. They also want to contribute to a better understanding of individual diseases: The scientists used skin cells from three patients with macrocephalic autism spectrum disorder to create stem cells, which they used to produce organoids and microglia cells. Past studies have revealed unusual behavior in neurons and microglia in patients with this disorder. The team has now shown that these differences also occur in the organoids.
“Our experiments showed that microglia in organoids derived from patients’ stem cells are more reactive to damaged cells than in organoids made with cells derived from control group individuals,” says Simon Schäfer. This change in behavior was also observed when microglia from the stem cells of the control group were seeded into brain organoids of patients. Consequently, this is more likely to be caused by changes in the brain environment rather than in the microglia’s own characteristics. This could explain the origin of the inflammatory processes in the brain often seen with this condition.
Brain, heart and pancreas as organoids
Simon Schäfer has been conducting research at TUM since 2022. His research group will participate in the interdisciplinary research of the Center for Organoid Systems, among other areas. Research on brain organoids is one of three core topics of the new center. In recent months other teams at TUM have published acclaimed studies on pancreatic and heart organoids.
“At TUM we will continue developing the brain model in order to find new links between the brain and the immune system,” says Simon Schäfer. “We also plan to develop stem cell-induced glial cells to make it possible to repair or replace tissue in case of brain damage.”
Schafer, S.T., Mansour, A. A., Schlachetzki, J.C.M., Pena, M., Ghassemzadeh, S., Mitchell, L., Mar, A., Quang, D., Stumpf, S., Santisteban Ortiz, I., Lana, A.J., Baek, C., Zaghal, R., Glass, C.K., Nimmerjahn, A., Gage, F.R. „An in vivo neuroimmune organoid model to study human microglia phenotypes“. Cell, Vol. 186 (2023): DOI: 10.1016/j.cell.2023.04.022.
- Prof. Simon Schäfer has been a professor at TUM since 2022. Before that he was conducting research with the team of Prof. Rusty Gage at the Salk Institute for Biological Studies in La Jolla, California. Essential parts of the research on this project took place there.
- Prof. Schäfer is a member of SyNergy, a Cluster of Excellence investigating the causes of complex neurological diseases such as multiple sclerosis and Alzheimer’s disease. With system neurology as a new interdisciplinary approach, the researchers can model the many processes involved in neurodegenerative, neuroimmunilogical and neurovascular diseases.
- The Professorship of Advanced Organoid Technologies for Mental Health Research was funded through the Hightech Agenda Bayern (HTA)
Technical University of Munich
Corporate Communications Center
- Paul Hellmich
- paul.hellmich@tum.de
- presse@tum.de
- Teamwebsite
Contacts to this article:
Prof. Dr. Simon T. Schäfer
Technical University of Munich
Klinikum rechts der Isar
Department of Psychiatry and Psychotherapy
Prorfessorship of Advanced Organoid Technologies for Mental Health Research
Tel: +49 89 4140 6661
simon.schafer@tum.de


![[Translate to en:] [Translate to en:]](/fileadmin/_processed_/1/a/csm__90A5680_2d82b2dda9.jpg)