Altered proteins trigger certain forms of dementia
Defective enzyme causes nerve cells to die
Central to this defense mechanism is the selenoenzyme glutathione peroxidase 4 (GPX4). A single mutation in the gene that encodes GPX4 can disrupt a crucial, previously unknown component of the enzyme’s function. In affected children, this leads to severe early-onset dementia. When fully functional, GPX4 inserts a short protein loop – a kind of “fin” – into the inner side of the neuronal cell membrane, enabling the enzyme to neutralize harmful substances known as lipid peroxides.
Surfing Along the Cell Membrane
“GPX4 is a bit like a surfboard,” says Conrad. “With its fin immersed into the cell membrane, it rides along the inner surface and swiftly detoxifies lipid peroxides as it goes.” A single point mutation found in children with early-onset dementia alters this fin-like protein loop: the enzyme can no longer insert into the membrane properly to perform its cell-protective function. Lipid peroxides are then free to damage the membrane, triggering ferroptosis and cell rupture, and the neurons die.
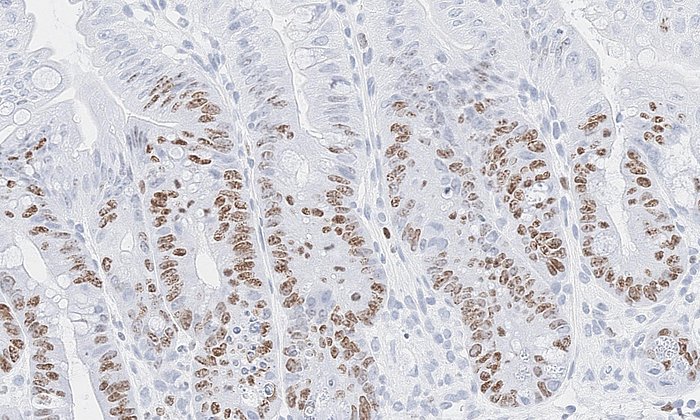
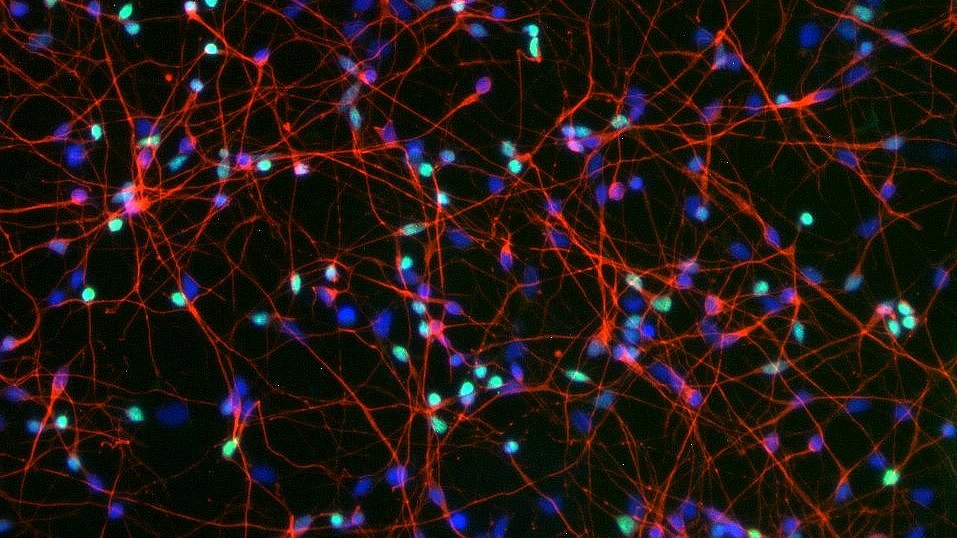
The study started with three children in the United States who suffer from an extremely rare form of early childhood dementia. All three carry the same change in the GPX4 gene, known as the R152H mutation. Using cell samples from an affected child, the researchers were able to study the effects of the mutation in more detail and reprogrammed the cells back into a stem-cell-like state. From these reprogrammed stem cells, they then generated cortical neurons and three-dimensional tissue structures resembling early brain tissue – so-called brain organoids.
Laboratory Evidence Confirms: Without Functional GPX4, Dementia Develops
To understand what happens at the whole-organism level, the team then introduced the R152H mutation into a mouse model, thereby specifically altering the GPX4 enzyme in different types of nerve cells. As a result of the impaired GPX4 function, the animals gradually developed severe motoric deficits, with dying neurons in the cerebral cortex and cerebellum, and pronounced neuroinflammatory responses in the brain – a pattern that closely mirrors the observations in the affected children and strongly resembles neurodegenerative disease profiles.
In parallel, the researchers analyzed which proteins change in abundance in the experimental model. They observed a pattern strikingly similar to that seen in patients with Alzheimer’s disease: numerous proteins that are increased or decreased in Alzheimer’s were likewise dysregulated in mice lacking functional GPX4. This suggests that ferroptotic stress may play a role not only in this rare early-onset disorder, but potentially also in more common forms of dementia.
A New View on The Causes of Dementia
“Our data indicate that ferroptosis can be a driving force behind neuronal death – not just a side effect,” says Dr. Svenja Lorenz, one of the first authors of the study. “Until now, dementia research has often focused on protein deposits in the brain, so-called amyloid ß plaques. We are now putting more emphasis on the damage to cell membranes that sets this degeneration in motion in the first place.”
Initial experiments also show that cell death triggered by loss of GPX4 can be slowed in cell cultures and in the mouse model using compounds that specifically inhibit ferroptosis. “This is an important proof of principle, but it is not yet a therapy,” says Dr. Tobias Seibt, nephrologist at LMU University Hospital Munich and co-first author. Dr. Adam Wahida, also a first author of the study, adds: “In the long term, we can imagine genetic or molecular strategies to stabilize this protective system. For now, however, our work clearly remains in the realm of basic research.”
Basic Research Helps to Understand Diseases at Their Roots
The study is the result of a research network that has grown over many years bringing together genetics, structural biology, stem cell research, and neuroscience, with several dozen scientists at multiple sites worldwide. “It has taken us almost 14 years to link a yet-unrecognized small structural element of a single enzyme to a severe human disease,” says Marcus Conrad. “Projects like this vividly demonstrate why we need long-term funding for basic research and international multidisciplinary teams if we are to truly understand complex diseases such as dementia and other neurodegenerative disease conditions.”
Lorenz S.M., Wahida A. et al. (2025): A fin loop-like structure in GPX4 underlies neuroprotection from ferroptosis. Cell (2025), DOI: 10.1016/j.cell.2025.11.014
-
Marcus Conrad is Professor of Translational Redox Biology at TUM and Director of the Institute of Metabolism and Cell Death at Helmholtz Munich.
-
Dr. Adam Wahida is a postdoctoral researcher at the Institute of Metabolism and Cell Death at Helmholtz Munich.
-
Dr. Svenja Lorenz is a post-doctoral researcher at the Institute of Metabolism and Cell Death at Helmholtz Munich.
-
Dr. Tobias Seibt is a specialist in internal medicine and nephrology at LMU Klinikum München.
Technical University of Munich
Corporate Communications Center
- Paul Hellmich
- paul.hellmich@tum.de
- presse@tum.de
- Teamwebsite
Contacts to this article:
Prof. Dr. Marcous Conrad
Technical University of Munich
Chair of Translational Redox Biology
marcus.conrad@tum.de