Overcoming resistance of pancreatic cancer to immunotherapies
“Inflaming” cold tumors

Pancreatic ductal adenocarcinoma (PDAC) is the most common form of pancreatic cancer. The disease is almost always fatal, with a 10-year survival rate of around 1 percent. The prognosis is especially poor for a subgroup of these tumors known as mesenchymal PDAC subtype, where even the strongest combination chemotherapies do not improve the poor clinical outcomes.
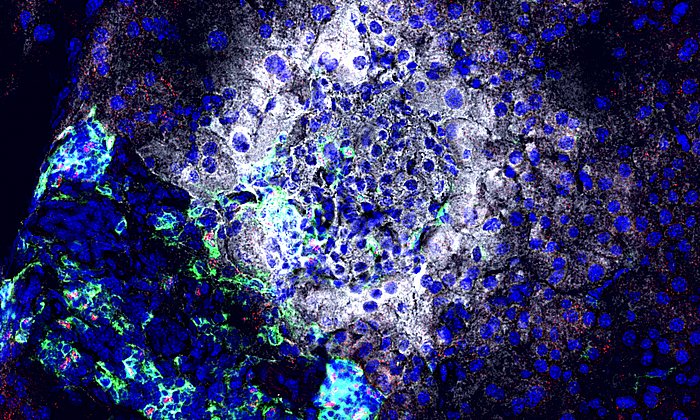
Mesenchymal PDAC is also unresponsive to modern immunotherapies such as checkpoint blockades. “There are different reasons for this. First, there are few features on the tumor cell surface that enable immune T-cells to identify them as “foreign”. Second, the nature of the microenvironment does not allow therapeutically active T-cells to infiltrate the cancer. We therefore call it an immunologically “cold” tumor,” says Dieter Saur, Professor of Translational Cancer Research at the Technical University of Munich (TUM). Saur is one of the scientists working at the Munich partner site of the German Cancer Consortium (DKTK) at the University hospital Klinikum rechts der Isar.
Improving the success of immunotherapies in treating pancreatic cancer
If this microenvironment could be reprogrammed to improve T-cell infiltration of the tumor, immunotherapy treatments would have a better chance of success. The scientists explored this hypothesis in a series of preclinical experiments in human pancreatic cancer cells and in mice.
The drug trametinib showed early promise with cancers that activate the RAF-MEK-ERK signaling pathway. Because pancreatic cancers of the mesenchymal subtype show the highest activation of this pathway, it appeared likely that a drug that inhibits this pathway could offer therapeutic benefits. Experiments showed, however, that treatments with trametinib alone were insufficient.
Promising combination therapies
The researchers therefore conducted high-throughput screening of 418 drugs on human PDAC cell cultures as well as cancerous cells from mice to find out whether one of them would improve the therapeutic effect of trametinib. They discovered that nintedanib, a drug already approved for lung fibrosis treatment, stimulated T-cells infiltration when used in combination with trametinib. “The combination of the two drugs led to cell cycle arrest and the death of cancerous cells. They also changed the microenvironment of the tumor,” says Dieter Saur, explaining the underlying mechanism.
Next the researchers investigated whether these changes could sensitize mesenchymal pancreatic carcinomes for treatment with immune checkpoint inhibitors. This question was explored through experiments on mice transplanted with tumor cells of PDAC subtypes. “The responses we observed in mice showed us that the anti-PD-L1 immunotherapy improved the effect of the combination treatment with trametinib and nintedanib,” says Chiara Falcomatà, the first author of the study. “The triple treatment significantly improved the response of the tumor, leading to a clear survival advantage of the highly aggressive mesenchymal PDAC subtype.”
Results are a first step toward targeted treatment
The results represent an important first step toward targeted treatment of mesenchymal PDAC, for which there are currently no efficient therapeutic options. The researchers believe that the combination treatment may also have the potential to create anti-tumor immunity with other cancer types, resulting in improved therapeutic outcomes.
Several authors of the current study are working at TranslaTUM, the Center for Translational Cancer Research at TUM. In this interdisciplinary research institute, doctors work with colleagues from the fields of natural sciences and engineering on research into causes and treatments of cancer.
Chiara Falcomatà, Stefanie Bärthel, Sebastian A. Widholz, Christian Schneeweis, Juan José Montero, Albulena Toska, Jonas Mir, Thorsten Kaltenbacher, Jeannine Heetmeyer, Jonathan J Swietlik, Jingyuan Cheng, Bianca Teodorescu, Oliver Reichert, Constantin Schmitt, Kathrin Grabichler, Andrea Coluccio, Fabio Boniolo, Christian Veltkamp, Magdalena Zukowsk, Angelica Arenas Vargas, Woo Hyun Paik, Moritz Jesinghaus, Katja Steiger, Roman Maresch, Rupert Öllinger, Tim Ammon, Olga Baranov, Maria S. Robles, Julia Rechenberger, Bernhard Kuster, Felix Meissner, Maximilian Reichert, Michael Flossdorf, Roland Rad, Marc Schmidt-Supprian, Günter Schneider and Dieter Saur: Selective multi-kinase inhibition sensitizes mesenchymal pancreatic cancer to immune checkpoint blockade by remodeling the tumor microenvironment. Nature Cancer 2022, DOI: https://www.nature.com/articles/s43018-021-00326-1
The German Cancer Consortium (DKTK) brings together the German Cancer Research Center (DKFZ) in Heidelberg, as the core center, and renowned cancer research institutions at German universities in long-term research partnerships.
The German Cancer Research Center (Deutsches Krebsforschungszentrum, DKFZ) with its more than 3,000 employees is the largest biomedical research institution in Germany. More than 1,300 scientists at the DKFZ investigate how cancer develops, identify cancer risk factors and search for new strategies to prevent people from developing cancer. They are developing new methods to diagnose tumors more precisely and treat cancer patients more successfully. The DKFZ's Cancer Information Service (KID) provides patients, interested citizens and experts with individual answers to all questions on cancer. Jointly with partners from the university hospitals, the DKFZ operates the National Center for Tumor Diseases (NCT) in Heidelberg and Dresden, and the Hopp Children's Cancer Center KiTZ in Heidelberg. In the German Consortium for Translational Cancer Research (DKTK), one of the six German Centers for Health Research, the DKFZ maintains translational centers at seven university partner locations. The NCT and DKTK sites combine excellent university medicine with the high-profile research of a Helmholtz-Zentrum. They contribute to the endeavor of transferring promising approaches from cancer research to the clinic and thus improving the chances of cancer patients. The DKFZ is 90 percent financed by the Federal Ministry of Education and Research and 10 percent by the state of Baden-Württemberg. The DKFZ is a member of the Helmholtz Association of German Research Centers.
Technical University of Munich
Corporate Communications Center
- Dr. Katharina Baumeister
- katharina.baumeister@tum.de
- presse@tum.de
- Teamwebsite
Contacts to this article:
Prof. Dr. Dieter Saur
Technical University of Munich (TUM)
Professor of Translational Cancer Research
dieter.saur@tum.de