Pediatrics: Ewing sarcoma tumor growth impeded in animal models
Researchers block gene activity in bone tumors
The five-year survival rate of children and adolescents with bone or soft tissue sarcomas is around 60 to 70 percent. This already represents a substantial increase in cure rates regarding these highly malignant tumors over the past few decades – thanks in particular to advances made by German physicians. However, children and adolescents are hit hard by the long-term effects of ablative surgery and toxic chemo- and radiotherapy. Moreover, the prognosis for patients with metastases or relapses remains significantly poorer.
Now, though, a TUM research group has identified new approaches for diagnosing and treating Ewing sarcoma – the outcome of a research project spanning several years, led by biochemist PD Dr. Günther Richter and oncologist Prof. Stefan Burdach from the Department of Pediatrics at the TUM University Hospital Klinikum rechts der Isar in cooperation with the Schwabing Children’s Hospital. Ewing sarcoma is the second most common type of bone cancer in children and young adults. It frequently affects the pelvis and long bones of lower extremities, but tumors can also originate in muscle, fat and connective tissue.
Transmission of genetic information blocked
Ewing sarcoma is caused by DNA double-strand breaks and their defective repair. A particular gene fuses with another gene at a different location in the chromosomes. This results in production of the oncofusion protein EWS-FLI1, which triggers tumor formation and growth.
TUM researchers have now managed to halt production of the oncofusion protein in a mouse model by significantly altering its underlying genetic activity. They achieved this using a specific molecule (JQ1) that blocks certain proteins such as BRD4. Without this protein, DNA to RNA transcription – that is, the transmission of genetic information – cannot take place to produce the oncofusion protein. This also induces cell death in existing tumor cells. With this method, the researchers were able to substantially reduce tumor growth and spread.
Low mutation rate
“These epigenetic findings provide us with new avenues to explore when developing therapies,” explains Richter. Results from basic research of this project also show the extent to which the development of cancer is influenced not only by changes in the genes themselves but also by genetic activities. In an investigation of tumor samples from over 100 patients across Germany, the researchers established that Ewing sarcomas exhibit a very low mutation rate – as is already familiar from other types of tumor occurring in children. “This finding clearly confirms that the pediatric cancer cannot be attributed solely to genetic changes and moreover, that novel targeted therapies are needed in cancer treatment of children and adolescents,” emphasizes Burdach.
Two proteins as candidate tumor markers
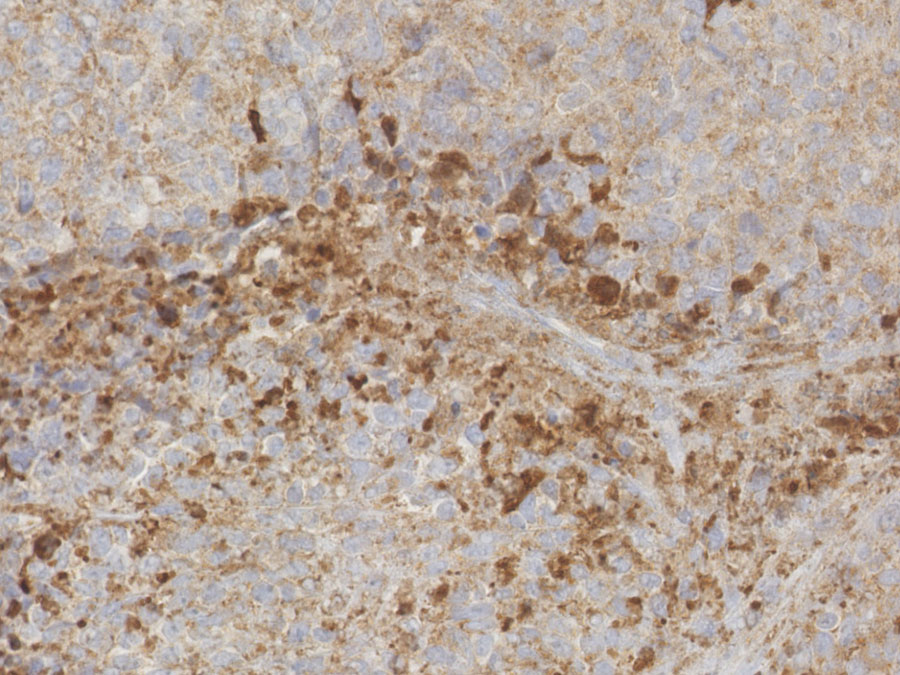
The TUM researchers also developed approaches for improved diagnosis of Ewing sarcoma. In their investigation of tumor samples, they identified two proteins as potential markers. They first determined that the DKK2 protein plays a key role in the infiltration and degradation of bone by the tumor cells. “We are currently performing tests within a Europe-wide study to confirm whether DKK2 is characteristic of invasive bone growth in Ewing sarcoma,” says Richter. Second, the GPR64 protein was also significantly upregulated. This occurs on the surface of the tumor cells and makes them resistant to cell death triggered by medication or lack of oxygen. So this protein is also a candidate for diagnosis.
Background:
The researchers are part of the Wilhelm Sander treatment unit for bone and soft tissue sarcomas at TUM University Hospital Klinikum rechts der Isar. The Wilhelm Sander Foundation is funding four research projects conducted by the group with the aim of improving diagnosis and developing individual therapies for patients with conditions not responsive to conventional treatment strategies. The Foundation supported the research project described here with funds of around EUR 170,000 over a five-year period.
Publications:
Hensel T, Giorgi G, Schmidt O, Calzada-Wack J, Neff F, Buch T, Niggli FK, Schäfer BW, Burdach S, Richter GHS (2016). Targeting the EWS-ETS transcriptional program by BET bromodomain inhibition in Ewing sarcoma. Oncotarget 7(2): 1451-63. DOI: 10.18632/oncotarget.6385
Agelopoulos K, Richter GHS, Schmidt E, Dirksen U, von Heyking K, Moser B, Klein HU, Kontny U, Dugas M, Poos K, Korsching E, Buch T, Weckesser M, Schulze I, Besoke R, Witten A, Stoll M, Köhler G, Hartmann W, Wardelmann E, Rössig C, Baumhoer D, Jürgens H, Burdach S, Berdel WE, Müller-Tidow C (2015). Deep sequencing in conjunction with expression and functional analyses reveals activation of FGFR1 in Ewing sarcoma. Clin Cancer Res. 21(21); 4935–46. DOI: 10.1158/1078-0432.CCR-14-2744
Richter GHS, Fasan A, Hauer K, Grunewald TGP, Berns C, Rössler S, Naumann I, Staege MS, Fulda S, Esposito I, Burdach S (2013). G-Protein coupled receptor 64 promotes invasiveness and metastasis in Ewing sarcomas through PGF and MMP1. J Pathol. May; 230(1): 70-81. DOI: 10.1002/path.4170
Hauer K, Julia Calzada-Wack J, Steiger K, Grunewald TG, Baumhoer D, Plehm S, Buch T, Prazeres da Costa O, Esposito I, Burdach S, Richter GHS (2013). DKK2 mediates osteolysis, invasiveness and metastatic spread in Ewing sarcoma. Cancer Res. 73(2): 967-77. DOI: 10.1158/0008-5472.CAN-12-1492
Contact:
PD Dr. Günther Richter
Technical University of Munich (TUM)
TUM University Hospital Klinikum rechts der Isar, Department of Pediatrics
Laboratory for Functional Genomics and Transplantation Biology, Children's Cancer Research Center
Phone: +49 89 3068 3235
guenther.richter@tum.de