Chemistry and medicine teams join forces to develop new strategies against prostate cancer
Gamma probe guides surgeons
Lymph nodes hosting prostate cancer metastases look quite innocuous initially. Since they measure no more than a few millimeters, they cannot be distinguished from their healthy neighbors with the naked eye. On top of this, metastases can also occur in lymph nodes located in parts of the body where doctors would not usually go looking for them. Even the standard imaging methods of magnetic resonance imaging (MRI) and computed tomography (CT) are not able to reliably identify these small metastatic lymph nodes.
An interdisciplinary team of researchers at TUM have now solved this problem by finding an effective way to make the cancer cells conspicuous. The key to the researchers’ solution is the PSMA (prostate-specific membrane antigen) protein. This protein occurs on the surface of cancer cells in prostate tumors and their metastases, but is otherwise rarely found in the human body.
Molecule binds specifically to metastases
The TUM researchers are developing different types of radiolabeled molecules, known as radioligands. Within the body, these bind specifically to proteins – in this case to PSMA, which are found on the cell surface of diseased tissue. If these labeled PSMA-binding molecules are injected into a patient’s bloodstream, they will bind to any metastases they find and emit radiation from there for a limited period. “Since we are working on a molecular scale, the patient will be exposed to just a very low level of radiation. Furthermore, the elements used have a short half-life and can only be detected in the body for anything between a few hours and a few days,” explains Prof. Hans-Jürgen Wester, Chair of Pharmaceutical Radiochemistry.
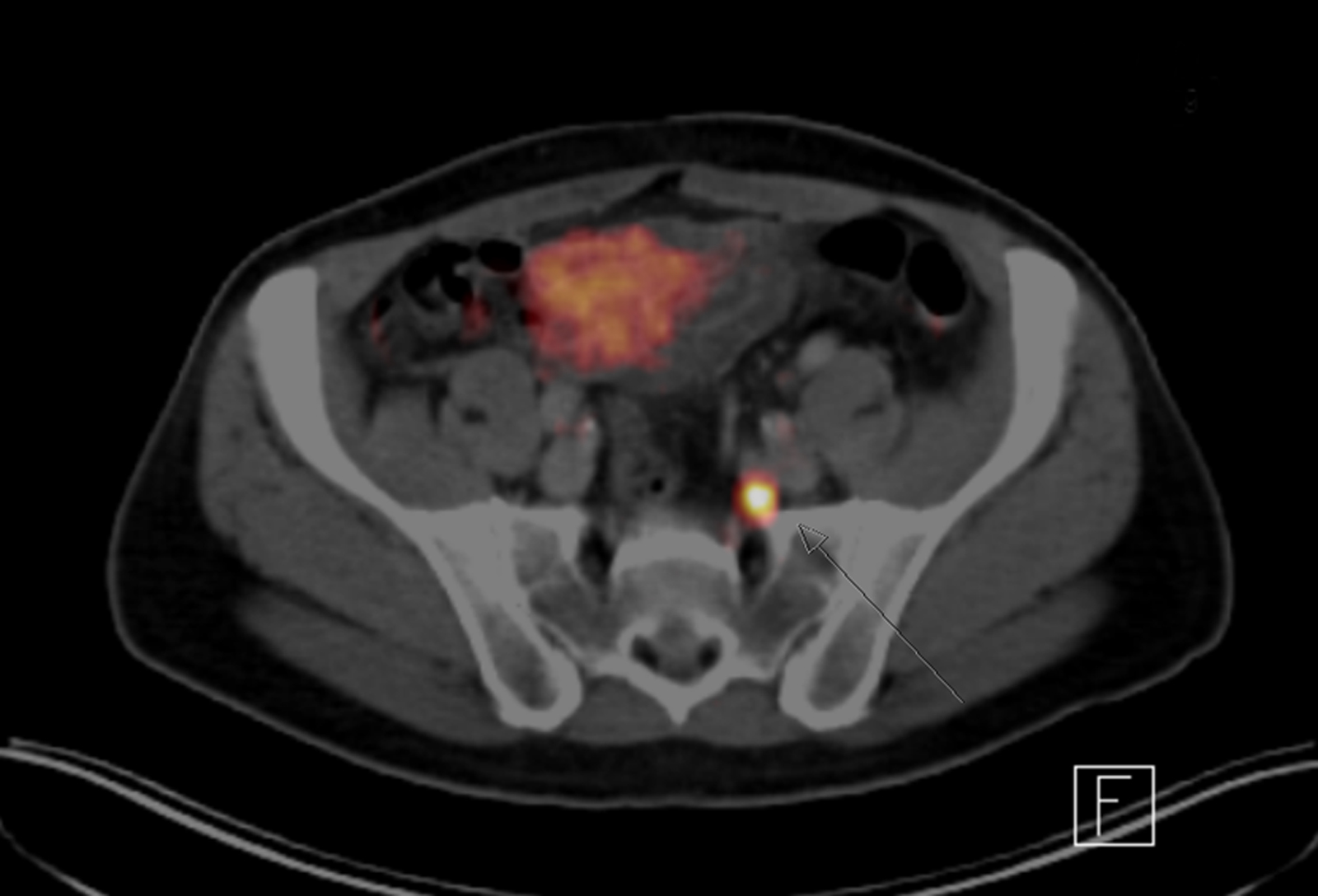
By using positron emission tomography (PET) combined with either CT or MRI the now radioactive metastases become visible and can be precisely located. TUM radiochemists, nuclear medicine scientists and urologists are working in close collaboration to develop and apply this method. Physicians will be able to infer from the data whether a surgical intervention would be expedient. They will then make the relevant decision in consultation with the patient, factoring in the results of the PET/CT scan but also considerations such as the patient’s physical state.
Gamma probe as target tracker
The ability to radiolabel metastases also opens up new possibilities for the removal of metastatic tissue. Physicians and researchers at TUM and the Klinikum rechts der Isar hospital have jointly developed an operative procedure called PSMA radio-guided surgery to this end. The day before the procedure, the patient receives an infusion with the PSMA radioligand. During the operation, the surgeon examines the tissue using a gamma-ray probe. Working in a similar way to a Geiger counter, the probe measures the radiation and gives the surgical team acoustic and visual feedback.
“This method allows us to specifically identify metastatic lymph nodes and safely remove them,” explains senior physician Dr. Tobias Maurer from the Department of Urology. With conventional procedures, there is a real possibility that the altered lymph nodes would never be discovered. “With this method, we have had some success in identifying and subsequently removing tumorous lymph nodes that were so small that they had not even been picked up beforehand by our PET/MRI scan,” adds Prof. Markus Schwaiger, Inhaber des Chair of Nuclear Medicine.
Promising results
Klinikum rechts der Isar has become a pioneer in the use of PSMA radio-guided surgery. Introduced in 2014, improvements are being made to the procedure all the time. To date, around 60 patients have been treated, with very promising results. Systematic follow-up examinations in a group of 21 patients have shown a reduction of over 90 percent in the biomarker for prostate cancer in ten of the patients. Twelve patients needed no further treatment during the follow-up period of almost one year.
“Our method could become established as a new and important line of action in the multidisciplinary approach to prostate cancer,” maintains Prof. Jürgen Gschwend, Director of the Department of Urology. If the prostate cancer comes back, even tiny metastases could be removed in suitable patients, who would thus in some cases be able to avoid subsequent hormone or radiation therapy. The procedure will have to be evaluated in the coming months and years. According to Gschwend, identifying the most suitable patients for this treatment will be one of the top priorities.
ContaCt
PD Dr. med. Tobias Maurer
Klinik und Poliklinik für Urologie
E-mail: tobias.maurer@tum.de
Tel.: +49-89-4140-2522
Publications
T. Maurer, K. Schwamborn, M. Schottelius, H-J Wester, M. Schwaiger, J. Gschwend, M. Eiber. "PSMA THeranostics Using PET and Subsequent Radioguided Surgery in Recurrent Prostate Cancer". Journal of Clinical Genitourinary Cancer May 2016. DOI: 10.1016/j.clgc.2016.05.020
T. Maurer, G. Weirich, M. Schottelius, M. Weineisen, B. Frisch, A. Okur, H. Kübler, M. Thalgott, N. Navab, M. Schwaiger, H.-J. Wester, J. Gschwend, M. Eiber. "Prostate-specific Membrane Antigen–radioguided Surgery for Metastatic Lymph Nodes in Prostate Cancer". European Urology 68 (2015). DOI: 10.1016/j.eururo.2015.04.034
M. Eiber, T. Maurer, M. Souvatzoglou, A. Beer, A. Ruffani, B. Haller, F.-P. Graner, H. Kübler, U. Haberhorn, M. Eisenhut, H.-J. Wester, J. Gschwend, M. Schwaiger. "Evaluation of Hybrid 68Ga-PSMA Ligand PET/CT in 248 Patients with Biochemical Recurrence After Radical Prostatectomy". Journal of Nuclear Medicine. May 2015. DOI: 10.2967/jnumed.115.154153