What mucins can do in medicine
Multi-purpose mucus
The natural lubricant made of mucous molecules – mucins – found in our bodies is more than just a mechanical protective layer, it also wards off bacteria and viruses. Oliver Lieleg, Professor of Biopolymer Materials at TUM, and his team develop mucin-based materials for medical applications. Here is a look at some of their selected projects.
Mucus for dry eyes
What it's about: The team developed a coating for contact lenses that reduces friction between the lens and the eye, thus helping to prevent damage to the cornea.
Why it's important: There are approximately four million contact lens wearers in Germany. However, for patients with dry eyes suffering from an insufficient natural protective lubricant film between the eye and the lens, wearing contact lenses can be uncomfortable and may even result in corneal damage. Lieleg's team responded by developing a coating from mucins which is only a few micrometers thick, transparent, and protects the eye from damage.
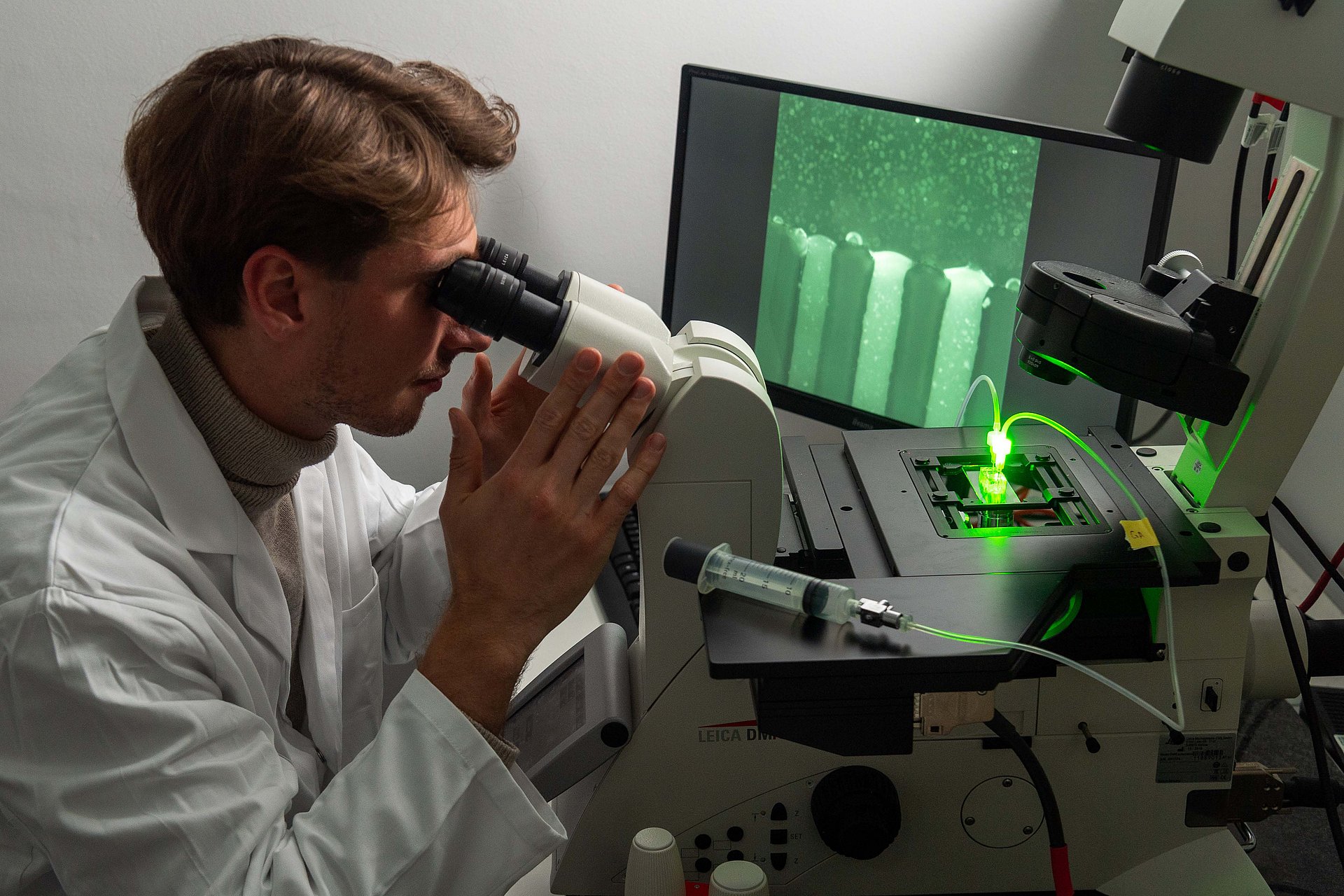
How it works: The team used specially purified mucins to coat both hard and soft contact lenses. The researchers tested the coated lenses in the lab on pig eyes. The coating improved the interaction of the lenses with water; and the researchers were able to show under the microscope that the porcine cornea remained intact even after stress tests with rubbing. The lenses stayed transparent and the mucin layer even made them resistant to the fat deposits that occur naturally in the tear fluid – otherwise, such deposits can result in clouding of the contact lenses after extended periods of use.
Publications: https://pubmed.ncbi.nlm.nih.gov/36521413/; https://pubs.acs.org/doi/10.1021/acsami.0c06847
Preventing respiratory tract damage
What it's about: The researchers have developed a mucin coating for endotracheal tubes to prevent tissue damage during in- and extubation.
Why it's important: Artificial respiration can save lives, but endotracheal tubes can also cause complications resulting from tissue damage or infection. An appropriate coating could reduce the risks involved in intubation.
How it works: The team used the same method to generate four different coatings on endotracheal tubes and compared the results. All the options tested (based on mucin, hyaluronic acid, polyethylene glycol, and lysine-dextran) reduced friction on tracheal tissue and prevented tissue damage. However, the mucin-based coating was much more efficient in preventing deposits of cells, bacteria, or fats.
Publication: pubs.rsc.org/en/content/articlehtml/2024/bm/d3bm01985c
Image: mediatum.ub.tum.de/1743393
Investigating the body's mucus layers
What it's about: The researchers use a model system to investigate what happens in the body's mucus layers when they come into contact with nano- or microparticles. For example, they tested if respirable dust has a negative impact on the protective effect of the mucus layer. They are also developing inhalable microparticle systems that release miniscule drug carriers specifically onto the mucus layer of the respiratory tract.
Why it's important: When we inhale tiny dust particles, pathogens or pollutants, the mucus layer in our respiratory tracts captures some of them. Thus, it is important for prevention, diagnosis, and medical applications to understand how harmful particles interact with the mucus layer. Moreover, the researchers are utilizing the moist properties of the mucus layer to package medications in such a way that they are released precisely at the mucus layer.
How it works: The researchers work with microfluidic chips, i.e., a model system in which they can study a gel made of mucins. This allows them to investigate the interfaces between the mucus layer and fluids, as in the intestines, and between the mucus layer and the air, as in the bronchia.
They used the model system to investigate what happens when the mucus layer is contaminated by respirable dust. "When the mucin layer contains respirable dust particles, its barrier effect is impaired. The tiny particles occupy molecular binding sites in the mucin gel which are intended to capture other molecules," says Oliver Lieleg.
In their latest project, the TUM researchers have been working together with scientists from LMU to develop tiny packagings for pharmaceuticals, which can be inhaled. Here they have designed small spheres (microparticles) which they can use to encapsulate even smaller drug carriers (nanoparticles). The charge and the structure of the microparticles determines their docking and decomposition process upon contact with the moist mucus. Among the various materials tested, the most successful one was the lysine packaging, since this positively charged amino acid performed best in binding to the negatively charged mucus.
Publication on inhalable drug carriers: https://doi.org/10.1002/anbr.202300153
Cooperation between TUM and Ludwig-Maximilians-Universität München (LMU)
Publication on respirable dust: https://pubs.acs.org/doi/10.1021/acsanm.2c03887
Images: https://mediatum.ub.tum.de/1743394
Closing and healing wounds
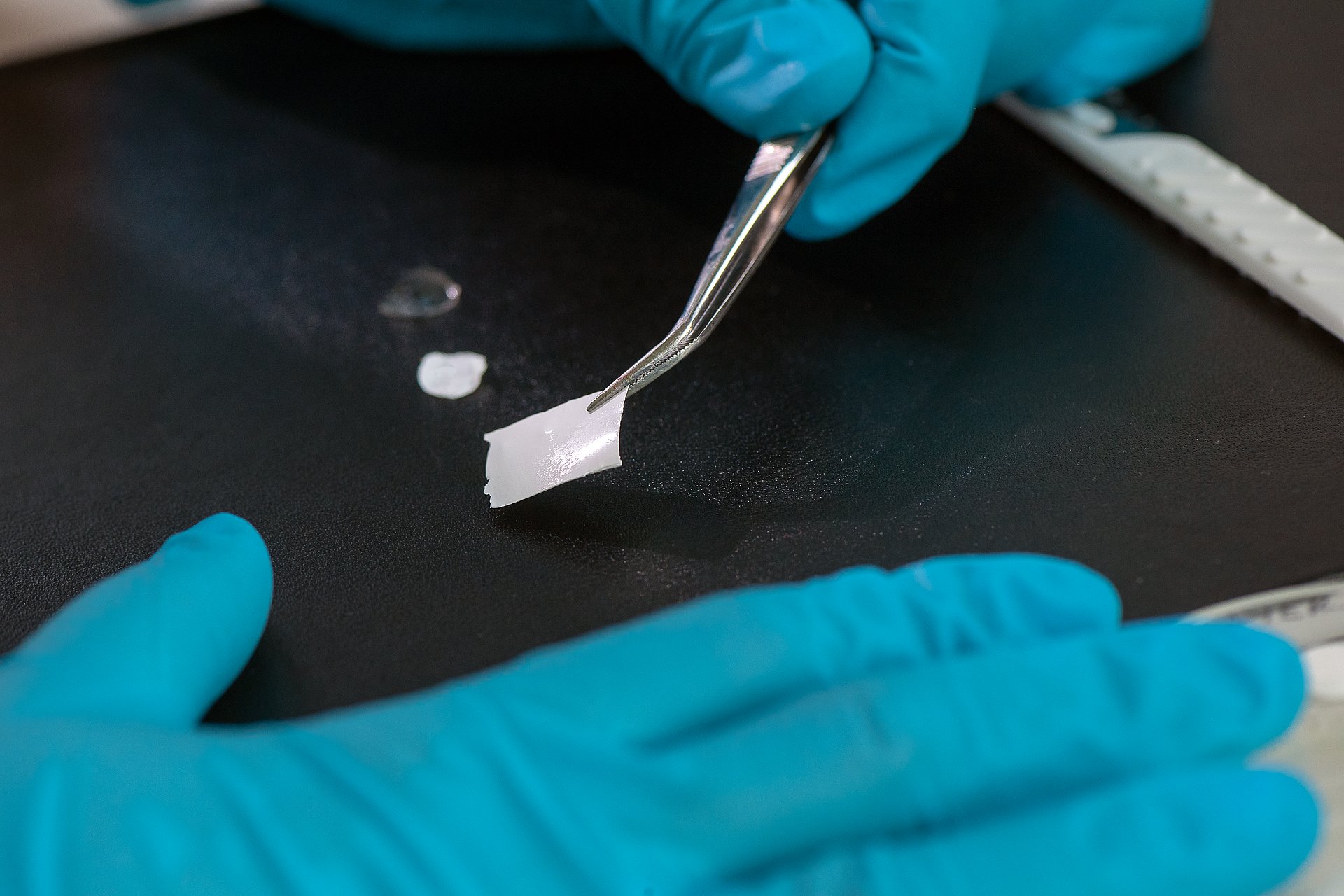
What it's about: Speeding up the wound healing process, dampening inflammation, and ultimately self-decomposing – a laboratory prototype of a multi-functional healing plaster based on mucins can do it all.
Why it's important: Conventional plasters are no use for treating injury to soft tissue such as the tongue or moist surfaces such as the intestine. This calls for an alternative: The mucin-based healing plaster adheres to moist soft tissue without damaging it, dampens inflammation, can release active ingredients in a directed manner, and then decomposes by itself after use. Self-decomposition can be particularly useful in the context of post-operative use to protect internal wounds that are no longer accessible after surgery has been completed.
How it works: The plaster consists of two layers. The top side contains the mucins which have an antibacterial effect. In addition, a biodegradable, synthetic polymer gives the plaster a certain amount of stability. The bottom layer contains among other things hyaluronic acid, known for its ability to bind water and promote wound healing, and dopamine. Dopamine ensures adhesion to moist tissue. The researchers can also integrate active ingredients such as antibiotics in the lower layer, which are then released towards the wound.
There is currently a prototype of the plaster for laboratory purposes. The team is now working on modifying the composition of the components in order to make the thin film more stable so that the plaster can be adapted to additional application cases. The researchers would also like to develop a wound-healing suture with a mucin coating for closing wounds.
Article: https://www.tum.de/en/news-and-events/all-news/press-releases/details/multifunktionales-pflaster-zur-wundheilung
Publication: https://doi.org/10.1002/adfm.202105721
Images: https://mediatum.ub.tum.de/1659268
What lies ahead?
The team has been developing and optimizing the materials over the course of several years and tests prototypes under laboratory conditions. They use these prototypes to assess their functionality in cell cultures or on animal tissue specimens. They are also investigating certain parameters like sterilizability, i.e., aspects that go beyond basic research but are necessary for a later application. Further steps and clinical studies leading to clinical approval will be necessary for future use of the applications on patients.
Video: Prof. Lieleg about his research
- Prof. Oliver Lieleg conducts research at the Munich Institute of Biomedical Engineering (MIBE), an Integrative Research Institute at TUM, and at the Center for Functional Protein Assemblies (CPA). At MIBE, researchers specializing in medicine, the natural sciences, engineering, and computer science join forces to develop new methods for preventing, diagnosing or treating diseases. The activities cover the entire development process – from the study of basic scientific principles through to their application in new medical devices, medicines and software.
This article was published in the 01/2025 issue of the new TUM Magazine.
Technical University of Munich
Corporate Communications Center
- Carolin Lerch
- presse@tum.de
- Teamwebsite
Contacts to this article:
Prof. Dr. Oliver Lieleg
Technical University of Munich
Professor of Biopolymer Materials
oliver.lieleg@tum.de