Rare disease: antisense RNA reduces seizures in premature infant
Treatment success in severe epilepsy
Many childhood epilepsies and developmental disorders have genetic origins. The case, recently published in Nature Medicine, involved SCN2A-related developmental and epileptic encephalopathy (SCN2A-DEE). This condition is caused by mutations in the SCN2A gene, which encodes a sodium channel essential for normal neuronal function. Mutations in the gene can lead to dysfunctional sodium channels, disrupting brain signal transmission. The result: early-onset seizures—often before three months of age—and profound developmental impairments.
In the Munich case, the SCN2A mutation was detected in utero through prenatal genetic testing. Such early diagnosis has become increasingly valuable with the emergence of personalized therapies. Pediatric neurology, which specializes in neurological disorders in children and adolescents, is at the forefront of this shift. Although available for only a small number of conditions so far, these innovative treatments hold promise—even as many clinical, technical, ethical, and logistical challenges remain.
RNA fragments prevent protein formation
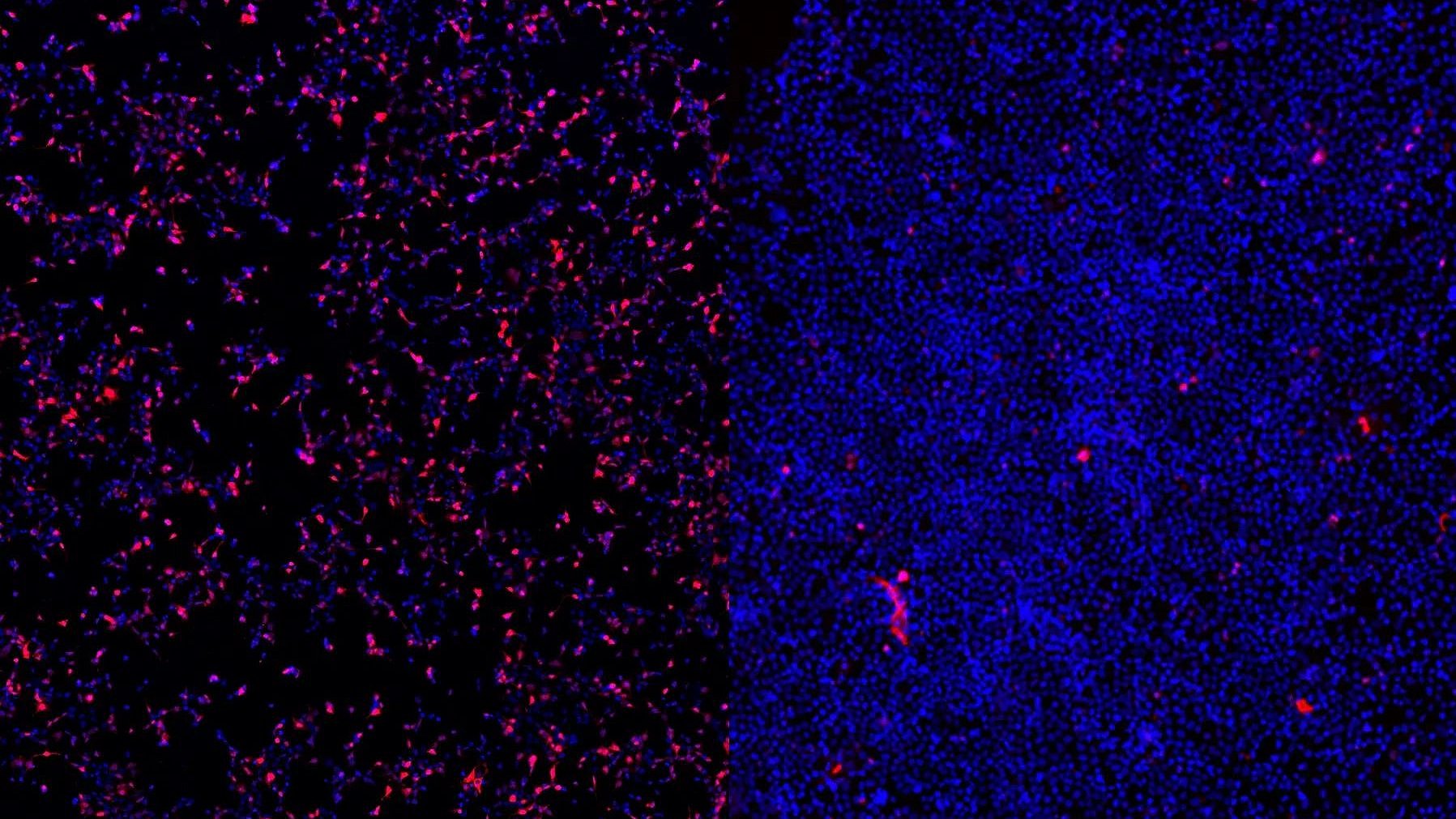
Antisense oligonucleotides (ASOs) are short strands of synthetic nucleic acids designed to bind specific RNA sequences. In precision medicine, ASOs are used to reduce or eliminate the production of disease-causing proteins. The ASO used in this case—named Elsunersen—targets the messenger RNA (mRNA) transcribed from the SCN2A gene. By binding to the mRNA and triggering its degradation, the faulty sodium channel protein is only produced at very low levels.
The physicians administered Elsunersen via intrathecal injection directly into the child’s spinal canal, alongside ongoing conventional therapy. The treatment interrupted the ongoing seizures and led to a sustained reduction—by more than 60%—to five to seven seizures per hour. This therapeutic effect lasted until at least 22 months of age and helped stabilize the child’s clinical care. However, severe developmental impairments persisted, likely due to the early and prolonged impact of the disorder during fetal development. Over the course of 20 months and 19 ASO administrations, no serious side effects were observed.
"Precision therapies are gaining in importance"
“This study highlights the potential of ASO therapies for genetic diseases,” says Dr Matias Wagner, head of the Nucleic Acid Therapeutics Group at the Institute of Human Genetics at the TUM University Hospital, and part of the LMU clinical team during the study. “In the future, we will both apply approved ASO drugs in precision medicine and evaluate new compounds in clinical trials. At the same time, we aim to develop tailor-made ASO therapies for patients who currently have no treatment options.”
“Antisense therapies mark a new era in epilepsy treatment,” adds Prof Ingo Borggräfe, head of the Pediatric Epilepsy Center at LMU Hospital. “Successful use requires extensive clinical experience, substantial logistical resources, and close interdisciplinary collaboration—all of which will continue to define our center’s mission in the years ahead.”
Building on this success, the Munich-based team plans to develop ASO-based treatments for other rare pediatric neurological disorders. These efforts will be integrated into comprehensive care models and benefit from the collective expertise of a cross-university research network.
Wagner, M., Berecki, G., Fazeli, W. et al. Antisense oligonucleotide treatment in a preterm infant with early-onset SCN2A developmental and epileptic encephalopathy. Nat Med (2025). DOI: https://doi.org/10.1038/s41591-025-03656-0
Contacts to this article:
Dr. Matias Wagner
Technical University of Munich
TUM University Hospital
Insitute of Human Genetics
Tel. +49 (0)89 4140 6381
matias.wagner@mri.tum.de
Prof. Dr. med. Ingo Borggräfe
LMU Klinikum
+49 (0)89 4400-57844
ingo.borggraefe@med.uni-muenchen.de